The IVF Process: Step-by-Step Guide for Intended Parents

Introduction to IVF (In Vitro Fertilization)
IVF (In Vitro Fertilization) is a revolutionary assisted reproductive technique that has provided hope and success to countless couples facing fertility challenges. This advanced medical procedure involves the meticulous combination of eggs and sperm outside of the human body within a controlled laboratory environment.
The resultant embryos are then transferred to the uterus, offering a promising route to achieving pregnancy for those in need. In this comprehensive guide, we’ll delve into the IVF Process details and address each phase.
Fertility-related awareness is not common like any other stream of healthcare. The lack of awareness makes it more difficult for couples who silently suffer from infertility or are sometimes not even aware of it.
Infertility is the inability of a couple to become pregnant even after one year of unprotected sexual intercourse using no birth control methods.
Any medical intervention that is done to assist a couple to have their own child can be considered an infertility treatment.
This can be as simple as receiving advice on the right time of the month to have regular sex, and as complex as a cycle of In-vitro fertilization. In layman’s terms, IVF means or IVF definition is to facilitate fertilization outside the body in a petri dish and then put the embryos back into the female uterus.
Get in touch for FREE SURROGACY CONSULTING:
Mobile: +91-8800481100 ( WhatsApp, Line, Viber)
Email: neelam@ivfconceptions.com
What is IVF?
IVF is a form of assisted reproductive technology (ART), which gives infertile couples a chance to have a biological child of their own.
In Vitro Fertilization (IVF) involves the mixing of a woman’s eggs and male sperm under an artificial condition in a laboratory and then transferring the resulted embryos to a woman’s uterus. The patients with the following conditions will be indicated for IVF.
- Male Factor Infertility
- Absent or Damaged Fallopian Tubes
- Endometriosis
- Unexplained Infertility
- Recurrent Intrauterine Insemination Failure
- Tubal and Pelvic Adhesions
- Preimplantation Genetic Diagnosis (PGD)
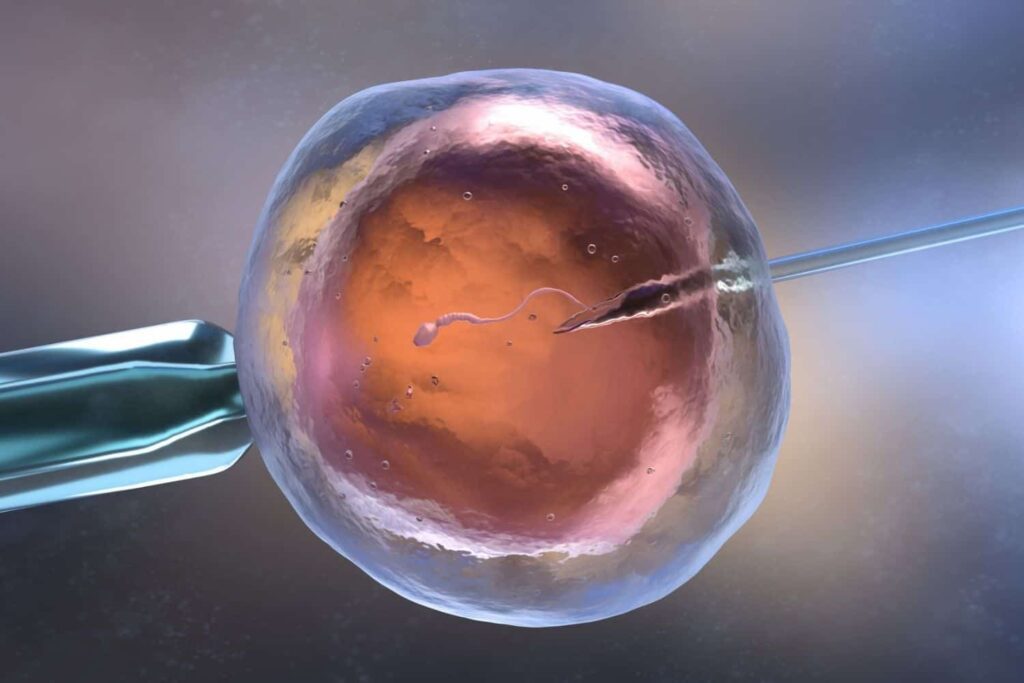
IVF-ICSI – Intracytoplasmic Sperm Injection, or ICSI, is a technique in which a single live sperm is injected into the center of a single human egg.
This technique is developed to help achieve fertilization for couples with severe male factor infertility or couples who have had a failure to fertilize in a previous in vitro fertilization attempt.
IVF-ICSI could be one of the best options for the couple struggling with male factor infertility, which includes low sperm count, low number of live sperm, sperm motility, and morphology issues. ICSI is also used to increase the success rate for unexplained infertility.
Generally, the fertilization rates with ICSI are 75%, which is the same as fertilization with a normal semen sample. The success rate of IVF and IVF with ICSI is the same; however, the current medical community believes that the success rate is better, maybe due to the higher number of fertilized embryos it yields, making it more popular among fertility experts.
Why Choose IVF?
Individuals and couples opt for IVF for various reasons, each stemming from a unique medical context. Infertility, caused by factors such as blocked or damaged fallopian tubes, endometriosis, or low sperm count, can prompt the decision to pursue IVF.
Moreover, IVF presents a viable solution for those with genetic disorders, offering the opportunity to screen embryos for health and compatibility. Same-sex couples and individuals who wish to conceive without a partner also benefit from IVF, which can provide the path to biological parenthood.
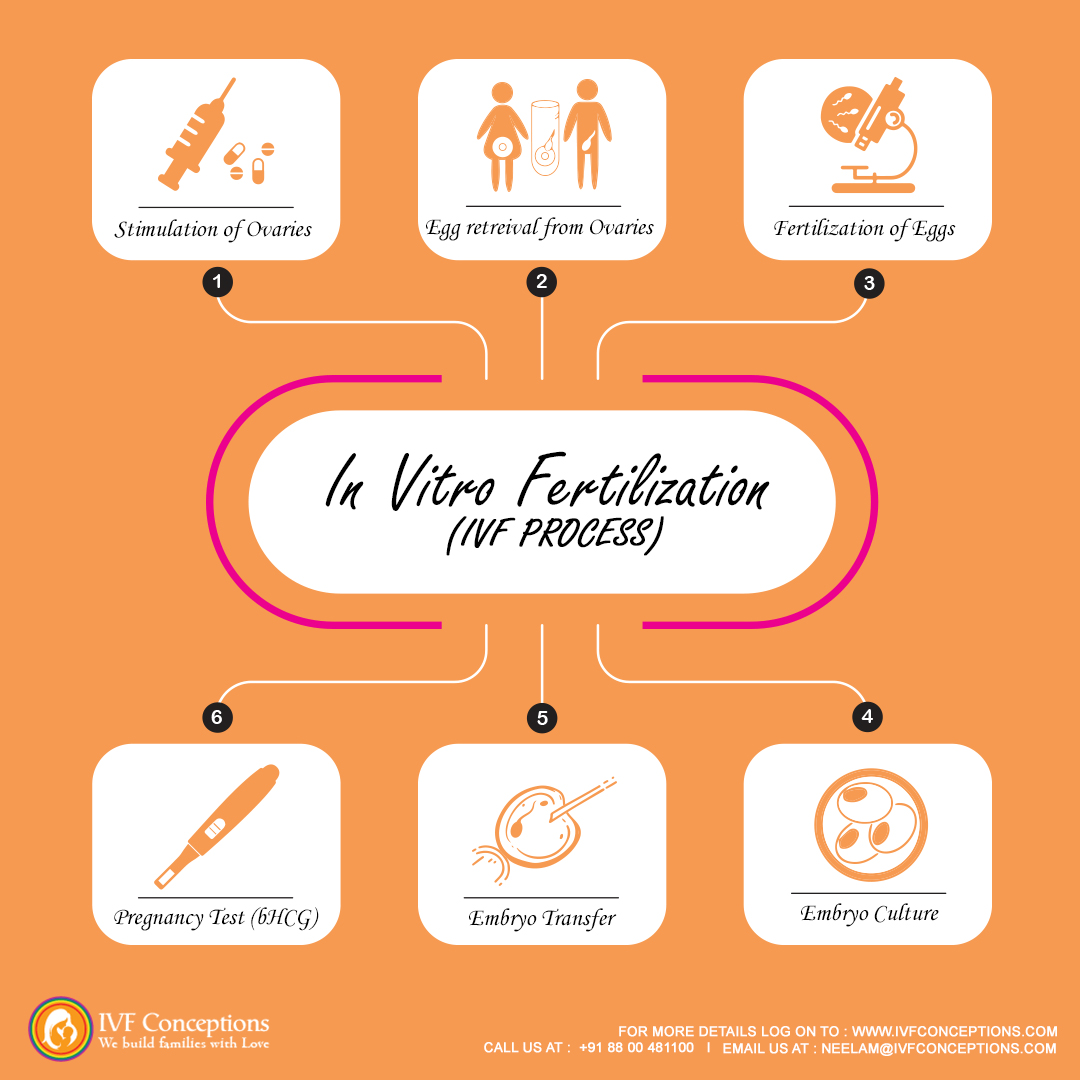
Step-by-Step IVF Process- In a nutshell
1. Ovarian Stimulation & Monitoring
- Goal: To produce multiple mature eggs for retrieval.
- Medications Used: Gonadotropins (FSH, LH), GnRH antagonists, and HCG trigger shots.
- Monitoring: Regular ultrasounds and blood tests to track follicle growth and hormone levels.
2. Egg Retrieval (Oocyte Collection)
- Procedure: A minor surgical procedure under sedation where mature eggs are aspirated from the ovaries using a thin needle.
- Recovery Time: 1-2 days with mild cramping or discomfort.
3. Sperm Collection & Preparation
- Collection Methods: Fresh ejaculation, frozen sperm, or surgical extraction (PESA/TESA) for male factor infertility.
- Sperm Processing: Sperm is washed and selected for the healthiest motile sperm for fertilization.
4. Fertilization & Embryo Development
- Methods:
- Conventional IVF: Eggs and sperm are combined in a petri dish for natural fertilization.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into an egg, often used for male infertility.
- Embryo Culture: The fertilized eggs develop into embryos over 3-5 days before transfer.
5. Embryo Transfer
- Timing: Usually performed on Day 3 or Day 5 (Blastocyst Transfer).
- Procedure: A catheter is used to place the embryo into the uterus under ultrasound guidance.
- Post-Transfer Care: Avoid strenuous activities and follow medication protocols.
6. Luteal Phase & Pregnancy Test
- Support Medications: Progesterone supplements to help implantation.
- Pregnancy Test: Conducted 10-14 days post-transfer to confirm implantation success.
Fresh vs. Frozen Embryo Transfer (FET)
| Factor | Fresh Transfer | Frozen Transfer |
|---|---|---|
| Timing | Immediately after retrieval | Postponed for optimal conditions |
| Success Rate | May be lower due to hormonal stimulation | Often higher due to better uterine preparation |
| Cost | Included in one cycle | Additional costs for freezing and thawing |
| Best For | Patients with high-quality embryos and a receptive uterine lining | Patients requiring further uterine preparation or PGS testing |
IVF Success Factors
Several factors influence the success of IVF:
- Age of the patient (Higher success in women under 35)
- Egg & sperm quality
- Uterine lining thickness
- Number of embryos transferred
- Lifestyle factors (BMI, smoking, stress levels)
Commonly Asked Questions (FAQs)
How many IVF cycles are typically needed?
On average, 2-3 cycles are required for successful pregnancy.
What are the risks of IVF?
- Ovarian Hyperstimulation Syndrome (OHSS)
- Multiple pregnancies (twins, triplets)
- Emotional and financial strain
What is the average IVF cost?
Costs range from $10,000 to $20,000 per cycle, depending on location, medication needs, and additional services like PGS testing or embryo freezing.

IVF costs in India and abroad
It goes without saying that having IVF babies or IVF babies is not easy to achieve. The IVF Cost is high, and it does not give a 100% desired outcome. The emotional and financial burden is not easy to handle for most couples.
Till now, infertile couples around the world are struggling to have affordable IVF treatments. Although in Asian countries like India, the IVF treatment cost in Delhi is still cheaper.
For some couples, using Third-Party Reproductive services like Egg donation IVF in Delhi and surrogacy is required to give them optimum chances of success. In such cases, the cost of overall infertility is much higher, as IVF, Egg donation, and IVF surrogacy is needed.
Although we offer IVF treatment in many countries, our aim is to give our lovely couples affordable IVF services in our IVF Clinic in Delhi, the cost of IVF is still low.
IVF Process- Step-by-Step Guide
The IVF treatment in Delhi involves multiple steps and can be done at a specific time of the female parent’s menstrual cycle. Although IVF is a costly treatment, it does not guarantee 100% success in pregnancy.
To have the optimum IVF Success rate, an experienced fertility doctor is needed, who can diagnose and provide the best line of treatment for childless couples.
An IVF treatment cycle typically includes the following steps:
Step 1. Suppressing the natural monthly hormone cycle
As a first step of the IVF process, you may be given a drug to suppress your natural cycle. To start this treatment, either a daily injection (which is normally self-administered unless you are not able to do this yourself) or a nasal spray is given. This continues for about two weeks.
Step 2. Increasing the Egg Numbers
After the natural cycle is suppressed, you are given a fertility hormone called FSH (or Follicle Stimulating Hormone). This is usually taken as a daily injection for around 10 to 12 days.
This hormone will increase the number of eggs you produce in each ovary. It means you will have more eggs to be fertilized with the sperm of the male partner and thus, many embryos for implantation.
With more fertilized eggs, the IVF clinic has a greater choice of embryos to use in your treatment. This means you can have more attempts for embryo transfer and so improved IVF success rates. Read more- IVF with an egg donor
Step 3. Checking on progress
Throughout the drug treatment, the clinic will monitor your progress for the number of follicles in the ovaries. The number and size of the follicles are closely monitored via vaginal ultrasound scans and blood tests.
Around 34 to 36 hours before your eggs are due to be collected, you have a final hormone trigger to help your eggs mature and subsequently get ready for retrieval.
Step 4. Collecting the eggs/semen sample
In the IVF process eggs are usually collected by ultrasound guidance under local anesthesia. This involves a needle being inserted into the scanning probe and into each ovary, facilitating egg pick up. Sometimes cramping and a small amount of vaginal bleeding can occur after the procedure.
The collection of sperm in the male partner is much easier. Around the same time when the female partner is going through the eggs collection procedure, the male partner is asked to produce a fresh sample of sperm.
This is stored for a short time before the sperms are washed and spun at a high speed. This is so the healthiest and most active sperm can be selected. If you are using donated sperm, it is removed from frozen storage, thawed, and prepared in the same way.
In case the childless couple is using an egg donor, the pre-IVF tests and stimulation and egg pick-up process are done with the egg donor.
Step 5. Fertilization of eggs with sperm
The eggs retrieved from the female partner are mixed with the male partner’s sperm under strict artificial conditions. The environment of the lab is closely monitored to give optimum chances of fertilization.
The embryos are cultured in the laboratory for 16 to 20 hours. A lab technician keeps a close look to check the fertilization rate.
Those that have been fertilized (now called embryos) are grown in the laboratory incubator for another one to two days before being checked again.
Step 6. Embryo Transfers
After fertilization, the best 1-2 embryos are selected and transferred to the female partner with the help of a thin catheter. This process can be done without anesthesia and takes 15-20 mins.
This process is known as embryo transfer and it is relatively simpler and does not require any anesthesia.
The number of embryos transferred is restricted because of the risks associated with multiple births.
The remaining embryos are frozen in vials for future use if this cycle is not successful. If not required immediately, frozen embryos can be kept for years. Or if not required, these embryos can be donated.
Some IVF clinics in Delhi may also offer blastocyst transfer ( Day 5 embryos), where the fertilized eggs are left to mature for five to six days and then transferred. This is known as Blastocyst transfer.
Step 7. Follow-up after Embryo Transfers
After embryo transfer, the recipient is asked to take 2 days of rest and avoid any strenuous activities. You need to take progesterone supplements continuously to support the implantation. Following 12 to 14 days of embryo transfer, blood tests known as the BHCG Serum test are done to confirm the pregnancy.
Step 8. Follow-up for pregnancy or next attempt
In case a successful pregnancy is confirmed through blood tests, continuous support of hormones is given until 10 weeks to 12 weeks.
If pregnancy is confirmed, then the rest of the antenatal care can be carried out like a normal pregnancy. In Scenarios where there is no pregnancy, further options are discussed with the couples.
In case you have frozen embryos stored, you can go ahead with frozen embryo transfer (FET). In case there are no surplus embryos, a new fresh IVF cycle is repeated.
If couples have multiple failed IVF cycles, your fertility doctor can suggest egg donor IVF for you.
ART-related terms for IVF Process
Frozen Embryos Transfer
Frozen embryo transfer (EFT) is a process in which frozen embryos are transferred to the uterus of the female partner, rather than fresh embryos.
Who is eligible to go through a frozen embryos transfer:
- This process can be useful when the couple is using donated embryos.
- If couples have surplus good quality frozen embryos left after the IVF cycle, and they wish to use them in the future.
- If the female partner does not have adequate lining as required for the embryo transfer, the doctor might decide to freeze the embryos and use them in subsequent months.
With the development of the latest technology, it is possible to freeze and store good-quality embryos on day 3 or blastocyst-stage with various freezing techniques.
Nowadays embryos are frozen using a vitrification technique; this process involves rapid freezing to prevent any ice crystals from forming in the cells of the embryo. The faster the freezing process, the more likely it is that a frozen embryo transfer will result in a successful pregnancy.
Frozen embryos can be stored for years. Although the chances of pregnancy are lower with frozen embryo transfer, the data is open to interpretation. When high-quality embryos are compared, there seems to be no difference in the likelihood of getting pregnant whether you have a fresh or frozen embryo transfer.
 Blastocyst Transfer
Blastocyst Transfer
Typically, while doing embryo transfer, Day 2 to Day 3 embryos are placed in the female partner’s uterus, and this is a procedure followed by most fertility clinics.
However, blastocyst embryo transfer is a process in which embryos are cultivated till day 5 in the lab, and then embryo transfer is done from Day 5 to day 6 after fertilization. By this time, the embryo reaches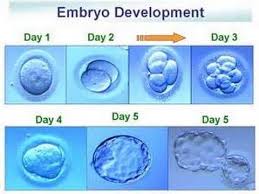 about 120-150 cells stage and is known as the blastocyst.
about 120-150 cells stage and is known as the blastocyst.
The benefits of Blastocyst Transfer are:
- A blastocyst can significantly reduce the chances of multiple births as only 1 or 2 good-looking embryos, which have survived till Day 5 in artificial conditions, are chosen and transferred.
- Nowadays most fertility clinics offer IVF with blastocyst transfer as it has been shown to improve success chances.
- A Blastocyst can withstand till day 5 in the lab and seems to be strong enough to survive. Thus parents can expect to optimize their success rate with it.
Embryo Donations
Embryo Donation and Embryo Adoption are similar concepts, and sometimes the terms are used interchangeably.
Both refer to the giving and receiving of embryos created during an In Vitro Fertilization (IVF) cycle. Once IVF has been done and is successful, the remaining embryos are frozen for future use. Or else, it can be donated to prospective Intended Parents or for scientific research.
However, the recipients’ intended parents have no genetic link with the baby and the female partner is the only gestational carrier of the child. So, embryo donation is like adoption; however, there is a more emotional connection as the female partner carries the baby for full pregnancy and subsequent delivery.
Few couples like to choose an egg donor and sperm donor of their choice to create embryos before the embryos are transferred to the female partner. In this case, couples have particular egg donor requirements and are ready to spend more on a new IVF cycle.
 Male Infertility
Male Infertility
Infertility is a widespread phenomenon at the current time. Not all fertility-related issues are women-oriented, as a matter of fact, there is a fundamental rise in male-related infertility issues. Out of 5 infertile couples, one of the couples is unable to conceive due to male-related fertility issues.
Male fertility is on the rise owing to stressful and sedentary lifestyles. The good news is that most infertility-related issues can be diagnosed and cured with the correct medical help
For males, the first line of assessment is via Sperm Analysis. It is a simple sperm analysis test that can indicate the quality and quantity of the sperm to a fertility specialist.
Male-related fertility issues
Male-related fertility factors are mostly due to low sperm counts, low sperm motility, abnormal morphology, no sperm at all, or some other genetic inherited condition.
Low Sperm count
Male infertility is a common factor nowadays due to an unhealthy lifestyle and excessive stress in the present time. In ART treatment like IVF-ICSI, even a few good sperms could be utilized to fertilize the eggs. There are a few medicines, and vitamin supplements, suggested to use before starting the IVF process.
Sperm Motility
Less sperm motility can cause hindrance in successful fertilization, and that is why IVF is used to rule out these male fertility issues.
Learn more about
Male-related infertility and how to manage it
Everything you need to know about Sperm DNA fragmentation
Birth Injury and link of Tylenol to ADHD and autism
Sperm Morphology
This factor is related to the abnormal shape of sperm, the head part, or the tail part. Generally, abnormal-looking sperms are seen under the microscope, but what needs to be analyzed further is their genetic makeup. There is a greater chance of having unsuccessful conceptions, and miscarriages with such sperm. DNA fragmentation is common in sperms with morphology defects.
Seminal Fluid
Sometimes thick seminal fluid is also a reason for infertility. It became difficult for the sperm to travel through the viscous liquid and thus no pregnancy was achieved. Various ART treatments are available to fix this condition.
Hormonal Imbalance
Male hormone imbalance also hinders successful conceptions. To rule out such a situation, a fertility specialist will make some tests, and hormonal imbalance can be corrected with regular medication.
Ejaculation issues
The ejaculation issue is due to a medical condition where the male partner is unable to ejaculate seminal fluid. Ejaculation issues can be due to the blocking of tubes or other structural defects in the male reproductive organ. In some cases, PESA is one of the methods by which fertility specialists obtain sperm samples via a minor surgical procedure.
Unexplained Infertility
Unexplained infertility is a common cause of infertility in both partners. All tests and clinical analyses or scans show no apparent issues in any partner, but still, couples are unable to conceive. Unable to have a baby due to unexplained infertility is the most frustrating situation for couples who are unable to conceive without any apparent reason.
In some cases, it is advised to go through genetic screening to rule out any underlying genetic defect in embryos, which might stop implantation or successfully grow the fetus.
Surgical Sperm Retrieval
Sometimes a male partner is unable to ejaculate sperm because of blocked tubes in their testes or because of any other condition, which prevents their sperm from being released. For such a situation, a minor surgical intervention is needed to extract the sperm. This is known as Surgical Sperm Retrieval.
Some form of surgical intervention is required for sperm retrieval from testicles before doing IVF with intracytoplasmic sperm injection.
There are various methods of removing sperm as below depending upon the individual case.
TESA (Testicular Sperm Aspiration)
TESA involves placing a needle attached to a syringe through the skin of the scrotum and merely sucking out the fluid inside the testicle.
PESA (Percutaneous Epididymal Sperm Aspiration)
PESA involves the same needle and syringe technique, but the needle is placed directly into the epididymis.
Perc biopsy (Percutaneous biopsy of the testis)
Perc biopsy is similar to TESA, but a larger needle is used. The needle used is a 14 gauge needle, usually used to biopsy testicular tissue, and it usually extracts a more significant number of sperms.
MESA (Microsurgical Epididymal Sperm Aspiration)
An open surgical sperm retrieval procedure that uses an operating microscope to locate the tubules of the epididymis precisely, so that large numbers of sperm are extracted.
The fertility-related treatment option for a male partner is as follows:
IUI ( Intrauterine insemination)
It is a fertility treatment that involves placing sperm inside a woman’s uterus to assist in fertilization. IUI aims to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization. This is the first line of treatment for infertility. If there is no success even after 3 rounds of IUI, the fertility expert might suggest you go for an IVF process.
IVF (In Vitro Fertilization)
It is a process of fertilization of eggs and sperm, manually, in a laboratory dish, and then transferring the embryo to the uterus of the female partner. It is useful for couples who have fewer numbers and a lower quality of sperm.
ICSI ( Intracytoplasmic Sperm Injection)
It is an advanced form of IVF that is used for the treatment of severe cases of male-factor infertility. It is done by manually injecting a good single sperm directly into a mature egg, thus facilitating fertilization. In the case of IVF, there can be a less fertilized embryo, but the idea behind the ICSI is to promote fertilization in as many eggs as possible manually.
Sperm Donor
In the rare case of extreme male infertility, the doctor will advise using a sperm donor. The sperm donor can be a young, healthy man who is used to fertilizing the female eggs so to achieve a successful pregnancy.
Addressing IVF Concerns and Considerations
Exploring the Risks and Benefits
As with any medical procedure, IVF is associated with its own set of risks and benefits. Multiple births, premature delivery, and the possibility of an ectopic pregnancy are potential risks. However, the success rate of IVF in achieving pregnancy remains a notable benefit.
It’s crucial for individuals and couples to engage in open dialogue with healthcare providers to make informed decisions tailored to their unique circumstances.
Navigating Emotional and Psychological Challenges
IVF encompasses not only physical aspects but also emotional and psychological facets. Individuals undergoing IVF may experience anxiety, depression, or feelings of overwhelming.
A strong support system, including healthcare professionals and counselors, plays a vital role in addressing these challenges and ensuring emotional well-being throughout the process.
 Maximizing Your IVF Journey
Maximizing Your IVF Journey
Factors Influencing IVF Success
Several factors impact the success of IVF, with age playing a pivotal role. Individuals under 35 years old tend to experience higher success rates, with live birth rates around 46%.
As age increases, these rates decrease, emphasizing the significance of timely intervention and consultation.
IVF Costs and Financial Considerations
While the average cost of an IVF cycle in the United States is approximately $15,000, this figure may vary based on individual health history, insurance coverage, and clinic-specific factors.
It’s imperative to discuss costs and explore available financial assistance options to ensure a comprehensive understanding of the financial implications of IVF treatment.
 Conclusion
Conclusion
If you are looking to have a low-cost IVF in Delhi with an optimum success rate, we are here to help. IVF Cost in India is much lower than in the rest of the world, with an excellent success rate.
We have built a relationship with multiple Best IVF Centers in Delhi and different countries, you can get the benefit of it by having world-class coordination services and a higher success rate.
If you’d like to learn more about IVF, Egg Donation, or surrogacy services globally, check out the rest of our website at IVF Conceptions. We offer legally secure and affordable surrogacy consulting services for FREE.
Get in touch now to get started! We recommend sending an email or filling out the forms below to know your best surrogacy options worldwide.
FAQs For IVF process step-by-step guide
- What is the IVF process?
The IVF (In Vitro Fertilization) process is an assisted reproductive technique where eggs are retrieved from the ovaries and fertilized with sperm in a laboratory setting. The resulting embryos are then cultured for a few days before being transferred into the uterus, aiming for a successful pregnancy.
- Who is a suitable candidate for IVF?
IVF is recommended for couples or individuals who face difficulties in conceiving naturally due to various factors like infertility, blocked fallopian tubes, male infertility issues, endometriosis, or unexplained infertility. A fertility specialist evaluates the specific case to determine suitability.
- How does IVF work?
IVF involves several steps: ovarian stimulation to produce multiple eggs, egg retrieval, fertilization of eggs with sperm in a lab dish, monitoring embryo development, and selecting viable embryos for transfer. The chosen embryo(s) are then transferred into the uterus, with hopes of implantation and successful pregnancy.
- What are the success rates of IVF?
IVF success rates vary depending on factors like age, overall health, and underlying infertility causes. On average, success rates range from around 20-40% per cycle. Younger individuals tend to have higher success rates due to healthier eggs.
- Are there any risks associated with IVF?
While IVF is generally safe, potential risks include ovarian hyperstimulation syndrome, multiple pregnancies (twins or more), ectopic pregnancy, and a slightly higher risk of birth defects. Consulting with a fertility specialist helps understand and manage these risks.
- How much does the IVF process cost?
IVF costs can vary significantly based on location, clinic reputation, medications required, and additional procedures. On average, a single IVF cycle can cost anywhere from $10,000 to $15,000 or more, not including medications.
- What medications are used during IVF?
IVF involves hormonal medications to stimulate the ovaries for egg production and prevent premature ovulation. Medications include gonadotropins, GnRH analogs, and hCG to trigger ovulation. These medications are tailored to each individual’s needs.
- How long does the IVF process take?
The IVF process typically spans several weeks. Ovarian stimulation takes around 8-14 days, followed by egg retrieval. Embryo culture lasts for 3-5 days, and embryo transfer occurs shortly after. The entire process from the start to the pregnancy test result can take 4-6 weeks.
- What is the role of a fertility specialist?
A fertility specialist, also known as a reproductive endocrinologist, is a medical doctor specializing in diagnosing and treating infertility and reproductive disorders. They guide patients through fertility treatment options, recommend personalized approaches, and oversee treatment cycles.
- Can I choose the gender of the baby through IVF?
Gender selection, also known as family balancing, can be achieved through IVF using a technique called preimplantation genetic testing (PGT). This method allows for the selection of embryos with a specific gender before implantation. However, it’s usually employed for medical reasons and may not be available in all situations or regions in India gender selection is not allowed
Reference used:
- https://www.eshre.eu (European Society of Human Reproduction and Embryology – ESHRE)
- https://en.wikipedia.org/wiki/Surrogacy (Wikipedia – General overview and country-specific laws)
- https://www.legislation.gov.uk (UK Government Legislation on Surrogacy)
- https://www.cdc.gov/art/index.html (Centers for Disease Control and Prevention – Assisted Reproductive Technology Data)


 Blastocyst Transfer
Blastocyst Transfer Male Infertility
Male Infertility

 Maximizing Your IVF Journey
Maximizing Your IVF Journey Conclusion
Conclusion