Infertility and Family-Building Acronyms, Explained.
In Assisted Reproductive Technology (ART), there are so many technical terms that have been used by fertility professionals and the community. This guide comprises a list of the most commonly used acronyms and definitions which you can refer to as and when needed during your fertility journey.
Let’s navigate through infertility and family-building acronyms.
Infertility affects many couples trying to start a family. Infertility is defined as the inability to conceive after a year of regular, unprotected intercourse. There are several possible causes of infertility, including issues with ovulation, problems with the uterus or fallopian tubes, and issues with the sperm.
When couples are struggling with infertility, they may turn to assisted reproductive technologies (ART) to help them build their family.
Get in touch for FREE SURROGACY CONSULTING:
Mobile: +91-8800481100 ( WhatsApp, Line, Viber)
Email: neelam@ivfconceptions.com


Let’s dive into the most commonly used- Infertility and Family-Building Acronyms

 AMH: Anti-Müllerian hormone
AMH: Anti-Müllerian hormone
Anti-Müllerian hormone (AMH) is a hormone produced by the cells that surround the immature eggs (follicles) in the ovaries of women. AMH levels are typically used as a marker of ovarian reserve, which refers to the number and quality of eggs remaining in the ovaries.
AMH levels can be measured with a simple blood test and it does not fluctuate during the menstrual cycle. High levels of AMH may indicate a higher ovarian reserve, while low levels may indicate a lower ovarian reserve.
This test can be useful in predicting a woman’s fertility potential and also in predicting the response to ovarian stimulation during assisted reproductive technology (ART) procedures such as in-vitro fertilization (IVF).
Learn more about- Learn everything about AMH and fertility
ART: Assisted Reproductive Technology
According to this definition given by CDC (Centers for Disease Control and Prevention ), ART includes all fertility treatments in which either eggs or embryos are handled. In general, ART procedures involve surgically removing eggs from a woman’s ovaries, combining them with sperm in the laboratory, and returning them to the woman’s body or donating them to another woman.
They do NOT include treatments in which only sperm are handled (i.e., intrauterine—or artificial—insemination) or procedures in which a woman takes medicine only to stimulate egg production without the intention of having eggs retrieved.
Additional Guides for Surrogate Mother:
Find a Surrogate Mother With or Without an Agency
In Which Country I Find Low-Cost Surrogate Mothers (in 2023)?
How can I Find a Surrogate Without Agency
What is the Age Limit for Surrogate Mothers
How Much Does Surrogacy Cost Using Family Member
How to Start the Gestational Surrogacy Process? A step-by-step guide for Beginners
How Much Does Surrogacy Cost? Everything You Need To Know (in 2023)
BBT: Basal Body Temperature
It is expected that the temperature will rise slightly around the time of ovulation. So, it is possible to track ovulation by taking temperature using a basal thermometer every morning before getting out of bed. Recording your temperature will help you learn if ovulation is taking place.

 BCP: Birth Control Pills
BCP: Birth Control Pills
Birth control pills are used to stop the monthly cycle and maintain the baseline condition of the uterine lining and follicles before starting IVF. Birth control pills are frequently used during fertility treatment and the egg donor and recipient cycles need to be synchronized. Also, if you are seeking fertility treatment aboard, and need to travel to start your IVF cycle, your doctor might like to control/manage your period by using birth control pills.
Beta: Beta HcG pregnancy test
Beta hCG pregnancy test is used to know the amount of hCG a woman has in her blood. hCG is produced by cells adjacent to the embryo and is measured 10 – 14 days after an embryo transfer. hCG levels increase every two to three days as your embryo continues to develop and generally, values double after 24 hours. To see the consistent fetus growth, your fertility doctor might repeat it 2 times.
CD: Cycle Day
Cycle day is the first day you have regular menstrual bleeding and continues until your new period arrives the following month. Most of fertility treatments are carried out based on the menses cycle of the women like Cycle Day 2 is when ovarian stimulation starts.
DE: Donor Eggs
If a woman is in a higher age group or unable to produce good eggs due to any medical condition, she is advised to use eggs from another lady, who is known as an egg donor, and the process is known as egg donation. Donor eggs can be frozen or fresh but most of the time fresh donor eggs are used for IVF. Learn, how to choose an egg donor.
DOR: Diminished Ovarian Reserve
This is a condition when women’s ovaries no longer produce a good quality and the number of eggs. It usually occurs with aging and menopause, but some genetic abnormalities, medical treatments, or injuries may also lead to an earlier DOR.
It is a common issue in women who come for infertility treatment as the age of conception is delayed due to professional commitments. For women with less ovarian reserves, egg donor IVF is advised.
ENDO: Endometriosis
Endometriosis is a condition when tissue that normally lines the uterus grows outside the uterus. Due to endometriosis, the tissue is can grow on the ovaries, fallopian tubes, or intestines.
The most common symptoms are pain and menstrual irregularities
ER: Egg Retrieval
It is a process that consists of the retrieval of the eggs from a woman’s ovaries for IVF and sometimes for egg-freezing purposes. This procedure is done under mild sedation and an ultrasound probe is inserted into the vagina and into each ovarian follicle. Gentle suction is used to retrieve the eggs one by one. The procedure takes 20-30 minutes with a short recovery time. Learn more about, the egg donation process.
As per Society for Assisted Reproductive Technology (SART), ‘it is common to have some vaginal spotting and lower abdominal distress for several days following the procedure.
ET: Embryo Transfer
The process of transfer of the embryo to the recipient’s uterus or surrogate mother’s uterus. This process of embryo transfer is easier than egg pick-up and does not require anesthesia.
FET: Frozen Embryo Transfer
This is a process when a frozen embryo either from the previous IVF cycles or a donated one is thawed and transferred into the intended mother’s or the gestational carrier’s uterus. Nowadays, most embryo transfers are frozen transfers as most of the intended parents choose to do genetic testing, where a biopsy is taken from the embryo on day 5 (blastocyst) and then frozen. Once they know which embryo is genetically healthy, the EFT process is started.
Related surrogacy Costs guides:
What is the average surrogacy cost?
How much does surrogacy cost in Ukraine?
How much does surrogacy cost in Georgia?
How much does surrogacy cost in India?
What is the Surrogacy Cost in Colombia?
What is Surrogacy cost in Mexico?
What is surrogacy cost with family members?

 FSH: Follicle-stimulating hormone
FSH: Follicle-stimulating hormone
The follicle-stimulating hormone helps regulate the menstrual cycle and stimulates the growth of eggs in the ovaries. FSH levels alter throughout the menstrual cycle, reaching a peak just before an egg is released by the ovary (ovulation). In men, FSH controls the production of sperm. It is seen that too much or too little FSH affects fertility.
hCG: Human Chorionic Gonadotropin
hCG is a hormone that is detected during pregnancy and it is produced by cells neighboring the embryo. hCG levels rise every two to three days as your embryo continues to develop and peak around the sixth week of pregnancy. It’s also the hormone detected by at-home pregnancy tests.
HSG: Hysterosalpingogram
A hysterosalpingogram is an X-ray-like process that is used to review the inside of the uterus and fallopian tubes, to check if the fallopian tubes are blocked and to see if the inside of the uterus is a normal size and shape.
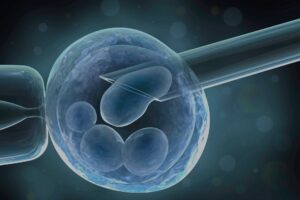
ICSI: Intracytoplasmic Sperm Injection
ICSI is an important part of the IVF process, where a tiny needle is used to inject a single healthy sperm into the center of the egg, under the guidance of a specially designed microscope. ICSI is the most used technique when there is a low number of sperm and if there is less sperm mobility. So, the fertility rate can be increased by ICSI and many fertility specialists prefer this process over normal fertilization.
IP: Intended Parent
It could be a couple or a single male or same-sex person, who becomes parents and is looking for the assistance of assisted reproductive technology such as IVF, IVF with an egg donor, surrogacy, or donor surrogacy.
IMSI: Intracytoplasmic Morphologically Selected Sperm Injection
Intracytoplasmic Morphologically Selected Sperm Injection (IMSI) is like intracytoplasmic sperm injection (ICSI) which is a widely used method in assisted reproductive technologies (ART) such as in-vitro fertilization (IVF).
The main difference between the two is that in ICSI, sperm is selected by the embryologist based on its movement and appearance, while in IMSI, the sperm is selected under high magnification (6000x) using a microscope that has the capability to distinguish between normal and abnormal sperm.
IMSI, like ICIS, is used for cases where there are sperm abnormalities such as low sperm count or poor sperm motility. The advantage of IMSI is that it allows for a more detailed selection of sperm, which may increase the chances of fertilization and improve the chances of a successful pregnancy.
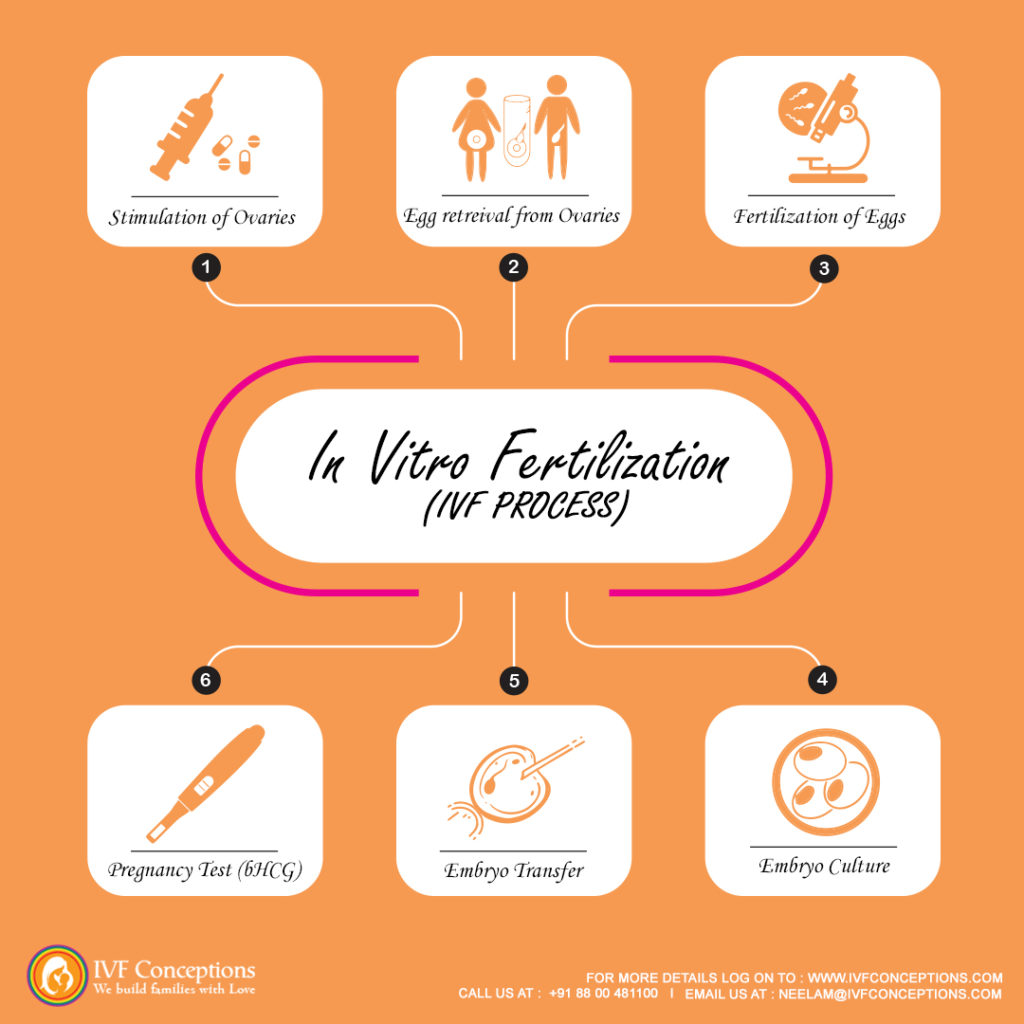
IVF: In Vitro Fertilization
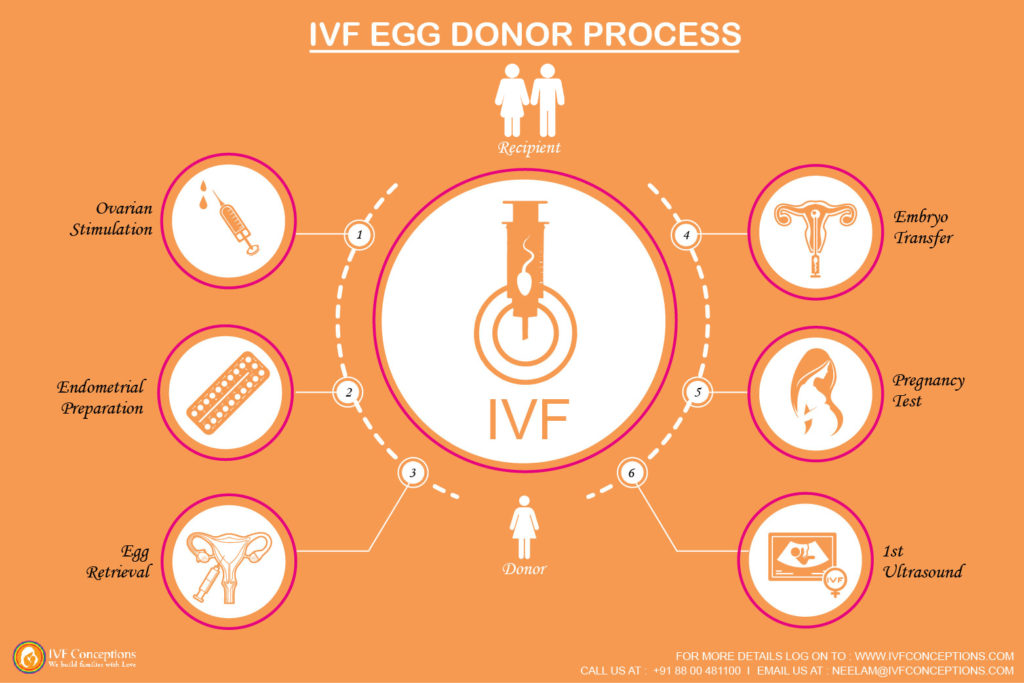
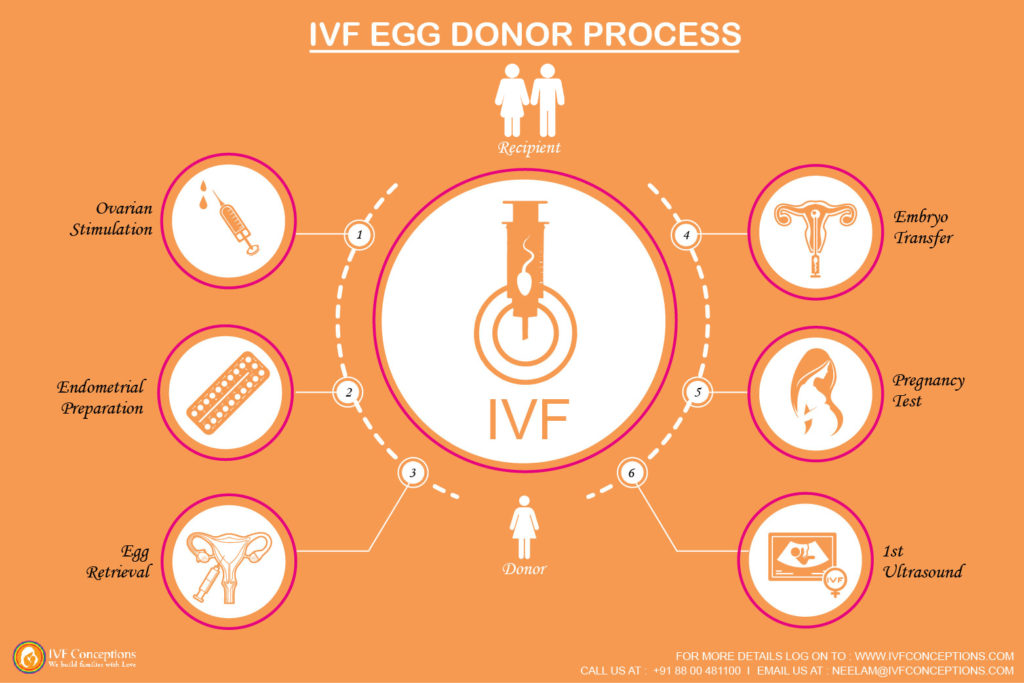
In vitro fertilization (IVF) is the most commonly used form of assisted reproductive technology (ART) that involves fertilizing an egg with sperm outside of the body. The procedure typically involves the following steps:
- Ovarian stimulation: The woman takes fertility medications to stimulate the production of multiple eggs.
- Egg retrieval: The eggs are retrieved from the woman’s ovaries using a procedure called transvaginal ultrasound aspiration.
- Fertilization: The eggs are fertilized with sperm in a laboratory dish, using a process called in vitro fertilization. This can be done by mixing the sperm and eggs together, or by using a procedure called intracytoplasmic sperm injection (ICSI), where a single sperm is injected directly into an egg.
- Embryo development: The fertilized eggs, now called embryos, are allowed to develop in the laboratory for several days.
- Embryo transfer: The embryos are transferred to the woman’s uterus, either one or more at a time, with the hope that one will implant and develop into a pregnancy.
IVF can be used for a variety of infertility issues, such as problems with ovulation, issues with the uterus or fallopian tubes, or issues with the sperm.
Read more: How does the IVF process work?
IVM: In vitro maturation
In vitro maturation (IVM) is a type of assisted reproductive technology (ART) that involves allowing immature eggs (oocytes) to mature outside of the body in a laboratory dish. The procedure typically involves the following steps:
- Ovarian stimulation: The woman takes fertility medications to stimulate the production of multiple eggs.
- Egg retrieval: The immature eggs are retrieved from the woman’s ovaries using a procedure called transvaginal ultrasound aspiration.
- In vitro maturation: The immature eggs are placed in a special culture medium and allowed to mature in the laboratory for 24-48 hours.
- Fertilization: The mature eggs are fertilized with sperm in a laboratory dish, using a process called in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI)
- Embryo development: The fertilized eggs, now called embryos, are allowed to develop in the laboratory for several days.
- Embryo transfer: The embryos are transferred to the woman’s uterus, either one or more at a time, with the hope that one will implant and develop into a pregnancy.
IVM is considered as an alternative to the traditional IVF procedure, especially for women with poor ovarian reserve. It’s important to note that IVM is not a guarantee of success and it’s important to consult with a specialist in reproductive medicine before starting any treatment. Additionally, IVM success rates are lower compared to traditional IVF and it’s still considered an experimental procedure.
IUI: Intrauterine Insemination
Intrauterine insemination (IUI) is a type of assisted reproductive technology (ART) that involves placing sperm directly into the uterus around the time of ovulation. The procedure typically involves the following steps:
- Ovarian stimulation: The woman takes fertility medications to stimulate the production of multiple eggs.
- Sperm preparation: The sperm is washed and prepared in the laboratory to separate the most motile sperm.
- Insemination: The prepared sperm is placed directly into the woman’s uterus using a thin catheter. This is typically done around the time of ovulation.
- Embryo development: If fertilization occurs, the fertilized egg will continue to develop and implant in the uterus.
IUI can be used for a variety of infertility issues, such as problems with the sperm, such as low sperm count or poor motility. It can also be used in conjunction with ovulation induction medications to increase the chances of conception.
Learn more: what is the difference between IVF and IUI?
LAP: Laparoscopy
Laparoscopic surgery checks for issues in the reproductive system. A thin surgical tube with a camera attached to it is inserted into the abdomen through a small incision.
It lets the surgeon view the body without major surgery and is used to diagnose and/or treat reproductive health issues, such as fibroids, ovarian cysts, and endometriosis.
LH: Luteinizing Hormone
Luteinizing hormone (LH) is a hormone produced by the pituitary gland in the brain. In women, LH plays an important role in ovulation, the process by which an egg is released from the ovary. LH levels rise just before ovulation, triggering the release of a mature egg from the ovary. This rise in LH is often referred to as the “LH surge.”
LH levels can be measured in a woman’s urine or blood. Ovulation prediction kits, which are commonly used to help couples time intercourse for conception, work by detecting the LH surge in the urine. In men, LH plays a role in the production of testosterone
LMP: Last Menstrual Period
LMP is the start date of one’s last menstrual period of women. Women who are undergoing infertility treatments are advised to note down their, LMP, menses date, etc to plan their treatment dates accordingly.
LSP: Low Sperm Count
Although even one sperm is enough to do the fertilization, despite this having a good number of sperm is required for the optimum success of IVF. Usually, when a patient’s sperm density is fewer than 15 million sperm per milliliter or less than 39 million sperm total per ejaculate.
As noted by the Mayo Clinic, normal sperm densities range from 15 million to greater than 200 million sperm per milliliter of semen.
MAI: Miscarriage after Infertility
A pregnancy loss after conceiving through fertility treatment.
MC, m/c, misc.: Miscarriage
When there is a spontaneous loss of a fetus before the 20th week of pregnancy. Miscarriages occur naturally – in about one in four pregnancies. A pregnancy loss beyond the 20th week is called a stillbirth.
MESA: Microsurgical epididymal sperm aspiration
Microsurgical epididymal sperm aspiration (MESA) is a surgical procedure that involves removing sperm from the epididymis, a small, coiled tube located behind the testicles.
The procedure is typically done in men who have a condition called obstructive azoospermia, which is the absence of sperm in the semen due to a blockage in the reproductive tract. This can be caused by a variety of factors, including injury, surgery, or congenital defects.
MESA is typically performed under general anesthesia and it is done by making a small incision in the scrotum. The epididymis is then visualized with a microscope and a small sample of tissue is removed.
The sperm is then extracted from the tissue and can be used for assisted reproductive technologies (ART) such as intracytoplasmic sperm injection (ICSI) where a single sperm is injected directly into an egg.
MF: Male factor
When the cause of infertility is due to the male partner. It could be low sperm count, low motility of sperm, etc. According to RESOLVE, 30% of infertility cases are related to male factor issues.
O, OV: Ovulation
Ovulation is the process by which a woman’s ovary releases an egg. The egg then travels through the fallopian tube, where it may be fertilized by sperm. Ovulation typically occurs once per menstrual cycle, around day 14 (in a 28-day cycle).
Understanding when you ovulate can help you plan a pregnancy or avoid one. Ovulation can be tracked by monitoring physical symptoms, such as basal body temperature or cervical mucus, or by using ovulation predictor kits.

 OB, OB/GYN: Obstetrician/Gynecologist
OB, OB/GYN: Obstetrician/Gynecologist
An Obstetrician/Gynecologist (OB/GYN) is a medical doctor who specializes in the healthcare of women, particularly in the areas of pregnancy, childbirth, and the reproductive system. They are trained to diagnose and treat issues related to the female reproductive system, including menstrual problems, infertility, and gynecological cancers. OB/GYNs also provide prenatal care, deliver babies, and perform cesarean sections (C-sections) if necessary. They also perform routine gynecological exams, such as pap smears, and breast exams.
PCOS: Polycystic Ovarian Syndrome
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders in women which affects fertility. It is characterized by the presence of multiple small cysts in the ovaries, which can lead to a variety of symptoms, including irregular menstrual periods, excess hair growth, acne, and weight gain. It is also associated with an increased risk of diabetes, high blood pressure, and heart disease. PCOS is a common endocrine issue that makes up 25% of infertility cases.
The exact cause of PCOS is not fully understood, but it is thought to be related to a combination of genetic and environmental factors. The condition is typically diagnosed based on the presence of certain symptoms, such as irregular periods, and high levels of androgens (male hormones) in the blood.
PGT-A: Preimplantation Genetic Testing for Aneuploidies
Previously known as preimplantation genetic screening (PGS), PGT-A provides detailed information about the embryo’s genetic health with the number of chromosomes. By knowing and selecting a healthy embryo for transfer, the chances of a successful pregnancy increase, and the chances of miscarriage decrease.
PGS: Preimplantation genetic screening
Preimplantation genetic screening (PGS) is a genetic test that is performed on embryos created through in vitro fertilization (IVF) before they are transferred to the uterus. The test looks for chromosomal abnormalities in the embryos, which can help identify those that are most likely to result in a successful pregnancy.
During PGS, a small number of cells are removed from the embryo and examined for chromosomal abnormalities. This can be done using a technique called fluorescent in situ hybridization (FISH) or more advanced methods like array comparative genomic hybridization (aCGH) or the next-generation sequencing (NGS) method.
PGS can help couples who have a higher risk of chromosomal abnormalities, such as advanced maternal age, recurrent miscarriage, or a family history of chromosomal disorders.
PGT-M: Preimplantation Genetic Testing for Monogenic Disorders
Previously known as preimplantation genetic diagnosis (PGD), PGT-M tests for hereditary disorders caused by mutations in a single gene, such as cystic fibrosis or Huntington’s disease.
PI: Primary Infertility
Primary infertility refers to the inability to become pregnant after trying for a certain period of time, usually one year if the woman is under 35 years old or six months if the woman is over 35 years old. This is the first time that a couple tries to conceive and it’s considered primary infertility.
The causes of primary infertility can be varied and can affect both men and women. Some common causes in women include problems with ovulation, such as polycystic ovary syndrome (PCOS); issues with the fallopian tubes, such as blockages or damage; and problems with the uterus, such as fibroids or endometriosis.
In men, common causes include low sperm count, poor sperm motility, or abnormal sperm shape. Other factors such as age, lifestyle, and environmental factors can also contribute to primary infertility.
PID: Pelvic Inflammatory Disease
PID is an infection of a woman’s reproductive organs, a complication often caused by STDs, such as chlamydia and gonorrhea when left untreated. Other non-sexually transmitted infections can also cause PID. PID can sometimes if left untreated, can lead to infertility.
POF: Premature Ovarian Failure
Women naturally experience reduced fertility around 40 years old but for those with POF, this happens earlier; in some cases, even as early as the teenage years.
RE / REI: Reproductive Endocrinologist
A reproductive endocrinologist is a medical doctor who specializes in the diagnosis and treatment of infertility and other reproductive disorders. They are trained in the field of reproductive endocrinology and infertility (REI), which is a subspecialty of obstetrics and gynecology. They use a combination of medical treatments, such as hormonal therapy and assisted reproductive technologies (ART), to help couples and individuals conceive and have healthy pregnancies. Some common procedures that a reproductive endocrinologist may perform include in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and egg freezing. They also work with patients who have endocrine disorders, such as polycystic ovary syndrome (PCOS), that affect their fertility.
RPL: Recurrent Pregnancy Loss
When a woman experiences two or more miscarriages. The ACOG recommends a thorough physical exam and testing after three repeated miscarriages.

 SA: Semen Analysis
SA: Semen Analysis
A semen analysis is a laboratory test that is used to evaluate the quality and quantity of a man’s semen and sperm. The test is typically performed on a sample of semen that a man provides by ejaculating into a cup, usually at a doctor’s office or a fertility clinic.
The semen sample is then sent to a laboratory where it is analyzed for various parameters, such as sperm count, motility (movement), and morphology (shape). The results of the semen analysis can provide important information about a man’s fertility and can help to identify any underlying conditions that may be affecting his ability to conceive.
Semen analysis is usually the first test performed when a couple is having trouble getting pregnant. A normal semen analysis result should have:
-Sperm concentration of at least 15 million sperm per milliliter.
-At least 40% of sperm should be moving.
-At least 4% of sperm should have a normal shape.
Learn more about – Lowe sperm count treatment and analysis
10 natural ways to Boost Male Fertility and improve sperm count
SART: Society for Assisted Reproductive Technology
The Society for Assisted Reproductive Technologies (SART) is a professional organization in the United States that represents and supports the field of assisted reproductive technologies (ART) such as in-vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI) and other ART procedures.
SART’s mission is to provide leadership and advocacy for excellence in the practice of ART, to promote education and research, and to enhance the awareness of the public and the profession of the safety and efficacy of these technologies.
SI: Secondary Infertility
Secondary infertility refers to the inability to become pregnant or carry a pregnancy to term after previously achieving a successful pregnancy. It can affect couples who have had one or more biological children, or individuals who have given birth or carried a pregnancy to term using assisted reproductive technologies (ART).
The causes of secondary infertility can be similar to those of primary infertility, such as problems with ovulation, issues with the fallopian tubes or uterus, or problems with sperm production or function.
Additionally, secondary infertility can be caused by conditions or factors that develop or occur after a first successful pregnancy, such as age, endometriosis, pelvic adhesions, or changes in weight.
Diagnosis of secondary infertility typically includes a review of the couple’s medical history, physical exams, and testing, such as semen analysis and ovulation monitoring.
Treatment options may include lifestyle changes, medication, surgery, or assisted reproductive technologies (ART), such as in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
STD: Sexually Transmitted Disease
A sexually transmitted disease (STD), also known as a sexually transmitted infection (STI), is a condition that is spread through sexual contact. STDs are caused by a variety of microorganisms, including bacteria, viruses, and parasites. STD is not related to infertility but if not treated can lead to infertility.
TL/TR: Tubal Ligation, Tubal Reversal
Tubal ligation, also known as “getting your tubes tied,” is a permanent form of female sterilization in which a woman’s fallopian tubes are cut, tied, or blocked to prevent eggs from reaching the uterus and sperm from reaching the eggs, thus preventing pregnancy.
The procedure can be performed through a small abdominal incision (laparotomy) or through the cervix (mini-laparotomy or hysteroscopic methods)
Tubal reversal, also known as tubal sterilization reversal, is a surgical procedure that aims to restore the function of the fallopian tubes after a tubal ligation. The goal of the surgery is to reattach the fallopian tubes so that the eggs can once again move through the tubes and be fertilized by sperm.
The success rate of tubal reversal varies depending on the method of tubal ligation, the length of the fallopian tubes remaining after tubal ligation, and the patient’s age.
TTC: Trying To Conceive
Trying to conceive, also known as trying for a baby, is the process of attempting to become pregnant through sexual intercourse or assisted reproductive technologies (ART).
A common term used mainly related to women/couples trying to become pregnant naturally or with the support of fertility providers.
TESE: Testicular sperm extraction
Testicular sperm extraction (TESE) is a surgical procedure that involves removing a small sample of tissue from the testicles to extract sperm. The procedure is typically done in men who have a condition called azoospermia, which is the absence of sperm in the semen. This can be caused by a variety of factors, including genetic disorders, injury, or surgery.
TESE is typically performed under local or general anesthesia, and it can be done in two ways:
- Micro TESE: Microscopically guided testicular sperm extraction. This technique is used when a man has non-obstructive azoospermia and there is no sperm in the semen.
- Open TESE: A small incision is made in the testicles to extract sperm directly. This technique is used when a man has obstructive azoospermia and there is no sperm in the semen.
V/VR: Vasectomy, Vasectomy Reversal
A vasectomy is a surgical procedure that is performed on men as a form of permanent birth control. The procedure involves cutting or blocking the vas deferens, the tubes that carry sperm from the testicles to the urethra so that sperm can no longer be ejaculated during sex. This prevents pregnancy by stopping the sperm from reaching the egg.
Vasectomy reversal, also known as vasovasostomy, is a surgical procedure that aims to reconnect the vas deferens tubes and restore the flow of sperm.
This list of Infertility and Family-Building Acronyms includes most of the terms used for fertility treatments, but it is not an exhaustive list. There are many more important terms and topics, that you can make yourself familiar with, please feel free to explore our site.
If you’d like to learn more about IVF, Egg Donation, or surrogacy services globally, check out the rest of our website at IVF Conceptions. We offer legally secure and affordable surrogacy consulting services for FREE.
Get in touch for FREE SURROGACY CONSULTING:
Mobile: +91-8800481100 ( WhatsApp, Line, Viber)
Email: neelam@ivfconceptions.com