Embryo Grading and IVF Success Rates- Your Comprehensive Guide

Embryo grading is a critical aspect of the in-vitro fertilization (IVF) process, and it plays a key role in determining the success rates of pregnancy. At IVF Conceptions, we understand the complexities surrounding embryo grading and its impact on your journey towards parenthood.
In this comprehensive guide, we will explore deep into the intricacies of embryo grading, decoding the cryptic numbers and letters that signify the quality of your embryos. Our goal is to equip you with the knowledge and insights necessary to make informed decisions on your path to a successful pregnancy.
Get in touch for a Free Surrogacy Consultancy:
📲 +91-8800481100 ( WhatsApp, Line, Viber)
The Significance of Embryo Grading
When you embark on your IVF journey, one of the critical moments is the assessment of your embryos’ quality. Embryo grading is the process by which embryos are evaluated based on their form and quality.
This evaluation employs a numerical and alphabetical scale, such as ‘4AB,’ to describe each embryo. Understanding what these grades mean is paramount in determining the likelihood of a successful pregnancy.
Pic Source: https://www.invitra.com/en/embryo-culture-up-to-blastocyst-stage/
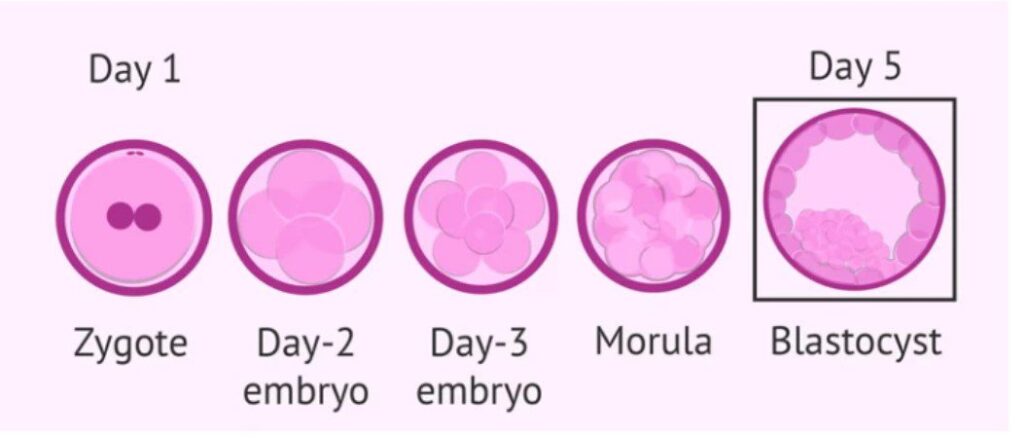
Embryo Development Stages
Before we dive into embryo grading, let’s briefly touch upon the different stages of embryo development, as this knowledge will help you appreciate the significance of grading.
- Zygote: This is where it all begins. When a sperm and egg meet, fertilization occurs, giving rise to a zygote.
- Compaction: Just before forming a morula, there’s a “compaction” stage where an 8-cell embryo undergoes transformations, becoming a solid ball of cells.
- Morula: This stage, occurring around four days post-fertilization, is a grouping of 12-15 cells resembling a blackberry and is the final phase before blastocyst development.
- Blastocyst: A blastocyst is a phase just before the embryo latches onto the uterine wall and “hatches” into a fetus, developing five days after fertilization. It consists of three distinct features: a round shell, a fluid-filled cavity, and an internal cell mass that will become the fetus.
- Hatching Blastocyst: Around six days after fertilization, a healthy blastocyst will hatch from its protective shell to implant in the uterine wall. Beyond this stage in the lab, the embryo is no longer viable.
The normal timeline for embryo development involves 2-4 cells by day two, 6-8 cells by day three, Morula formation by day four, and blastocyst development by day five or six. By day seven, the blastocyst should start hatching, and once hatched, the embryos are not viable for transfer.
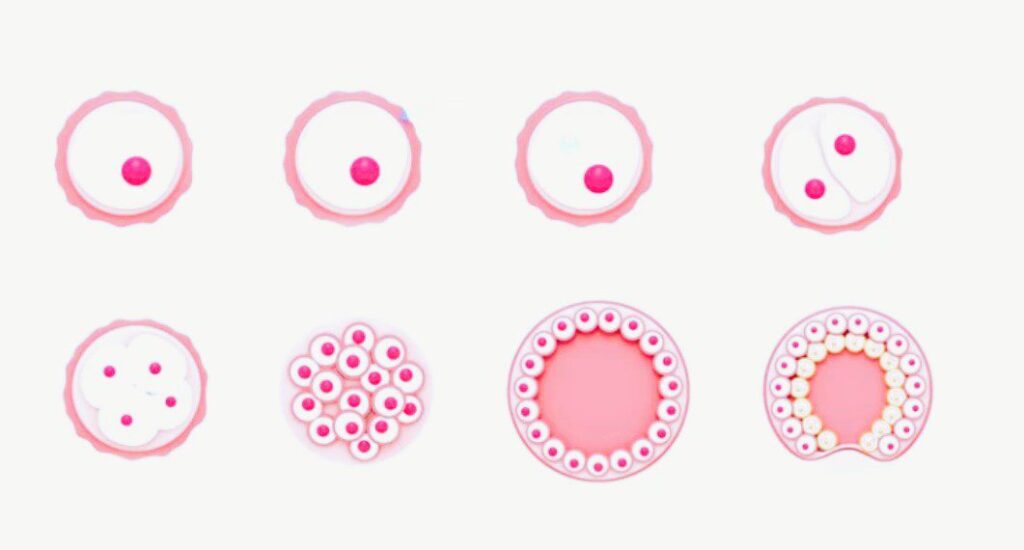
Understanding Blastocyst ( Day 5 Embryos) Quality
An important factor in embryo grading is the quality of the blastocyst, which plays a pivotal role in predicting the success of pregnancy.
A blastocyst is distinguished by its two clearly defined cell components and a fluid cavity. As it develops, these structures divide and expand.
The Inner Cell Mass (ICM) becomes the fetus, while the Trophectoderm (TE) becomes the placenta. Both must be well-formed for a successful pregnancy.
To assess the quality of blastocysts, the Gardner grading system is commonly used. It assigns three separate quality scores to each blastocyst:
- Blastocyst Development Stage: Ranging from 1 to 6, with 5 indicating the most developed stage.
- Inner Cell Mass (ICM) Score: Categorized as A to C, with A being the best.
- Trophectoderm (TE) Score: Also rated as A to C, with A representing the highest quality.
The most advanced blastocysts fall into the level 4 or 5 range, typically with letter grades of A or B. These are highly desirable for successful pregnancy outcomes.
More reference for Embryo Grading & IVF Success Rates::
Can Single Embryo Transfer Result in Twins?
Number of Embryos to Transfer in Surrogacy
Embryo Transfer Day: Guide to the Procedure, Process, and Tips
Should I Have PGS Testing on My Embryos?
How does the IVF embryo grade system work?
The embryo grade system considers the development in two stages. The day 3 embryo, also known as the “cleavage stage” embryo, looks at the number of cells and their structure, and the day 5 stage embryo (known as blastocyst) looks at the blastocyst stage.
To assess the quality of blastocysts, the Gardner grading system is commonly used. It assigns three separate quality scores to each blastocyst:
Blastocyst Development Stage: Ranging from 1 to 6, with 5 indicating the most developed stage.
Inner Cell Mass (ICM) Score: Categorized as A to C, with A being the best.
Trophectoderm (TE) Score: Also rated as A to C, with A representing the highest quality.
The most advanced blastocysts fall into the level 4 or 5 range, typically with letter grades of A or B. These are highly desirable for successful pregnancy outcomes.
The Gardner Embryo/Blastocyst Grading System is a common way embryologists grade embryos to determine embryo development and eventually possibility for success.
The system has three parts, a letter and two numbers (e.g. 4AA, 2BA, 5AB).
Let’s walk through each part:
- Blastocyst development stage: 1 – 6 (with 5 being the most developed)
- ICM quality: A – C (A being the best)
- TE Quality: A – C (A being the best)
The Number Part Means:
Let’s start with the numbers, 1-6. This number shows the blastocyst development stage or the score of the expansion of the embryo’s cavity.
- 1: Early blastocyst—the blastocele is less than half the volume of the embryo.
- 2: Blastocyst—the blastocele is greater than or equal to half of the volume of the embryo.
- 3: Full blastocyst—the blastocele completely fills the embryo.
- 4: Expanded blastocyst—the blastocele volume is larger than that of the early embryo and the zona pellucida is thinning.
- 5: Hatching blastocyst—the trophectoderm has started to herniate through zona pellucida.
- 6: Hatched blastocyst—the blastocyst has completely escaped from the zona pellucida.
The Letter Part Means:
After the number comes two letters. These letters are for the two parts of a day-5 embryo (also called a blastocyst):
- The Inner Cell Mass (ICM), which becomes the fetus
- The Trophectoderm (TE), which becomes the placenta and other essential tissues
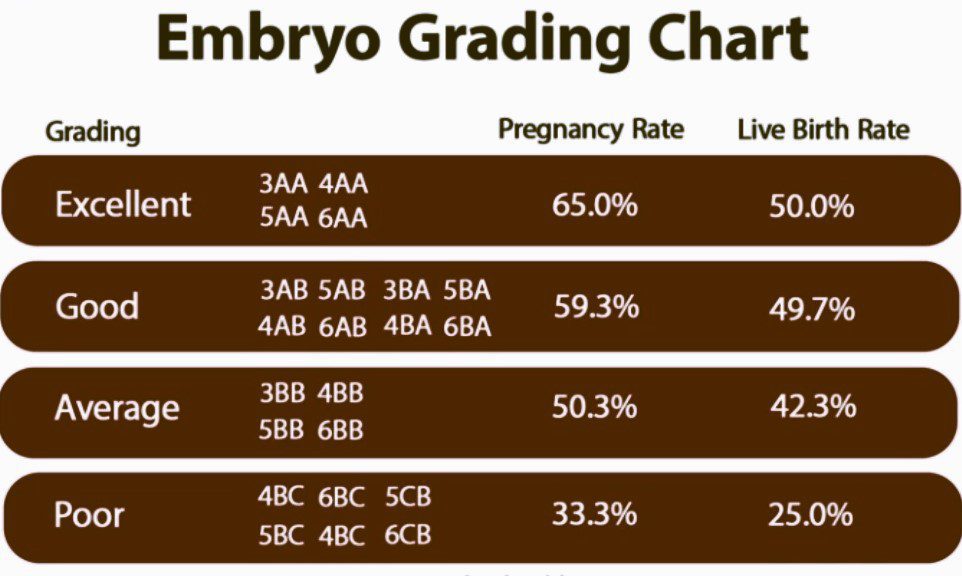
The Impact of Embryo Grade on Pregnancy Success Rates
Now that we’ve deciphered the intricacies of embryo grading and blastocyst quality, let’s explore how these factors influence success rates in your surrogacy journey.
Excellent Grade Blastocysts (e.g., 3AA or better):
These embryos exhibit the highest likelihood of success, with clinical pregnancy rates reaching approximately 65%. Embryos in this category include:
- 3AA
- 4AA
- 5AA
- 6AA
Good Grade Blastocysts (e.g., 3AB or better):
Embryos categorized as “good” had a 59.3% pregnancy rate and 49.7% live birth rate. Embryos in this category include:
- 3AB
- 4AB
- 5AB
- 6AB
- 4BA
- 5BA
- 6BA
Average Grade Blastocysts (e.g., 4BB, 4AC, 4CA, 2AB, 2BA):
While still promising, the pregnancy rate drops to around 50%. Embryos in this category include:
- 3BB
- 4BB
- 5BB
- 6BB
Poor Quality Blastocysts (e.g., 3BC, 4CB, 4CC, 2BB):
These embryos have a lower chance of success, with a pregnancy rate of just 33%. Embryos rated “poor” include:
- 4BC
- 5BC
- 6BC
- 4CB
- 5CB
- 6CB
The chart below illustrates the various blastocyst grades and their relative likelihood of leading to a successful pregnancy:
It’s essential to remember that embryo quality is just one aspect of the equation. Success in surrogacy also depends on the preparation of your surrogate and the expertise of the embryologist.
Nevertheless, understanding the quality of your embryos, as indicated by their grades, provides valuable insights into your surrogacy journey’s potential.
Early-Stage Transfers and Day 3 Embryos
While most ART cycles opt for blastocyst transfers on day 5, some clinics choose to transfer embryos during the earlier stages, typically on day 3. The rationale behind this strategy is that embryos may develop more optimally in the uterus, increasing the chances of reaching a healthy blastocyst stage.
During the early stages, embryos are graded differently, using an A, B, C, or D scale. This rating reflects the rate of development on that particular day, fragmentation percentage, synchrony of cell division, and evenness of cell division. These factors play a crucial role in determining the embryo’s overall quality.
At IVF Conceptions, we believe that informed decisions lead to successful surrogacy journeys. By understanding the nuances of embryo grading and success rates, you are better equipped to navigate the path to parenthood with confidence.
Conclusion
Embryo grading is a vital component of your IVF journey, offering insights into the quality of your embryos and their potential for a successful pregnancy.
At IVF Conceptions, we are committed to providing you with the knowledge and support needed to make informed choices on your surrogacy journey. We understand that the road to parenthood can be challenging, but with the right information and guidance, you can increase your chances of achieving your dreams of becoming parents.
Get in touch for a Free Surrogacy Consultancy:
📲 +91-8800481100 ( WhatsApp, Line, Viber)

FAQs for Embryo Grading & IVF Success Rates
Certainly, here are concise answers to your questions:
How is embryo grading determined?
Embryo grading is determined based on form and quality, typically using a number and two letters to describe each embryo.
What is the significance of blastocyst development in IVF?
Blastocyst development signifies advanced embryo development and readiness to implant in the uterine wall.
How does inner cell mass quality impact IVF success?
Inner cell mass (ICM) quality is significant in IVF as it determines the potential for the ICM to develop into the fetus.
What role does trophectoderm quality play in embryo grading?
Trophectoderm (TE) quality plays a key role in embryo grading by assessing the potential of TE to become the placenta and essential tissues.
Is embryo grading the sole predictor of IVF success?
Embryo grading is important but not the sole predictor of IVF success. Other factors like the skill of the embryologist and the preparation of the surrogate also play vital roles.
What is Preimplantation Genetic Testing for Aneuploidy (PGT-A)?
Preimplantation Genetic Testing for Aneuploidy (PGT-A) is a genetic screening method used to identify chromosomal abnormalities in embryos before implantation.
How do “excellent” graded embryos differ from “good” graded ones?
“Excellent” graded embryos typically have higher success rates and are more advanced in development compared to “good” graded embryos.
What are the success rates for embryos graded as “average”?
Embryos graded as “average” have moderate success rates, usually around 50% in achieving a pregnancy.
Can embryos with “poor” grading lead to successful pregnancies?
Embryos with “poor” grading may still lead to successful pregnancies, but their success rates are lower, approximately 33%.
Reference us:

